Robotic Knee Replacement
The use of robotic technology has several benefits.
- Improved accuracy and precision – There is always a small chance of human error in any operative procedure, robotic assistance adds an extra level of accuracy and precision to the surgery1-4.
- Increased consistency – In conjunction with being more precise, robotic technology is more consistent than conventional methods5.
- Less destructive and intrusive – The surgery can be performed through smaller incisions reducing the likelihood that patients will experience pain from ligament and soft tissue releases around the knee.
- Greater chance of restoring movement and mobility – As a result of a smaller incision, less soft tissue releases and greater accuracy of implantation many patients experience reduced recovery periods as well as an increased chance of restoring freedom of movement and complete mobility.
These benefits result in improved outcome metrics
- Better patient outcomes – It has been shown that patients who receive robotic surgery report better functional outcomes and experience fewer readmissions to hospital. They also require less rehabilitation than patients who undergo conventional knee replacement.
- Higher patient satisfaction – patients can return to their daily activities and work sooner after robotic knee surgery and this translates into improved patient satisfaction ratings.
- Lower long-term costs – Patients who receive robotic knee surgery tend to have fewer complications meaning less return visits to hospital. The CORI robotic system is an image free preoperative mapping system eliminating the cost and implications of a CT scan6. Patients also recover quicker and are able to get back to work sooner.
Is Robotic knee replacement surgery better?
Yes. Robotic surgery has been shown to deliver better results compared to conventional knee replacement. Improved accuracy, consistency and less bone and soft tissue trauma following a CORI robotic knee replacement result in better patient outcomes.
If the arthritis within the knee affects more than one compartment then a total knee replacement may be recommended.
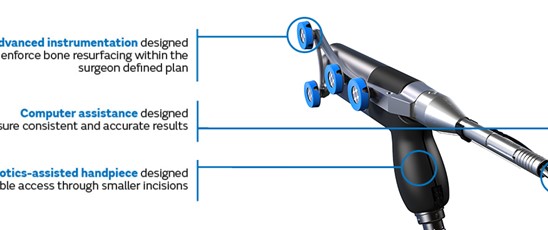

Unlike other robotic systems with the CORI robotic assisted total knee replacement there is no need for further imaging scans such as a CT and therefore radiation exposure is reduced. During a CORI robotic assisted total knee replacement the knee is mapped during surgery using a probe. Tracers can monitor the movement and stability of the knee and an accurate 3D model of the knee is created by the robot. Using this information, the robot can display the optimal sizing and positioning for the implants to enable a balanced, full range of motion. With this level of accuracy, the longevity, function and feel of the knee implant can be improved.
Video provided courtesy of Smith and Nephew
Through a midline incision the surfaces of the bone can be replaced. The femoral component is a smooth metal component of varying sizes, which fits over the end of the femur. The tibial component consists of a metal base plate that sits on top of the tibia and a polyethelene (plastic) insert that fixes onto the tibial component. The patella surface may be replaced if it is worn. The implants are positioned and fixed to the bone using bone cement.


You will be admitted on the day of surgery having not eaten for the preceding 6 hours prior to the operation (nil by mouth). The anaesthetist will talk to you regarding the type of anaesthetic (spinal or general anaesthetic), it is preferable to have a spinal anaesthetic as there are fewer side effects, improved pain control and a speedier rehabilitation whilst in hospital. See FAQ section spinal or general anaesthetic.
After surgery patients generally remain inpatients for 1-3 days. Patients mobilise full weight bearing on the same day of their surgery and generally go home with a stick or crutch for 1-2 weeks. After 4-6 weeks the vast majority of patients will have seen a significant improvement in their knee function.
Risk of Surgery
Common
- Bleeding – Bruising following the surgery is common, very occasionally a blood transfusion or iron tablets may be required. Rarely, the bleeding may form a collection within the knee joint which may require a further operation to remove it.
- Blood Clots – Deep vein thrombosis (DVT) is a blood clot in a vein. The risk of developing a DVT is greater after surgery (especially lower limb surgery). A DVT can pass in the blood stream and become lodged in the lungs causing a pulmonary embolus (see below). To limit the risk of DVTs forming you will be given stockings to wear on your legs whilst an inpatient and a daily tablet or injection to thin the blood. Moving early after surgery is one of the best ways to prevent blood clots from forming.
- Pain – The knee will be sore after the operation. Pain will improve with time and generally is much improved by the 2 week post-operative mark. Rarely, pain can be a chronic problem.
- Knee Stiffness – This may occur after the operation, especially if the knee is stiff before surgery. If this continues for some time, despite physio input, a manipulation under anaesthesia may be recommended.
- Implant wear and loosening – With modern operating techniques and new implants, knee replacements last in excess of 20 years. In some cases they can fail and this is often as a result of the plastic liner wearing out.
Less Common
- Infection – You will receive antibiotics just before the operation starts and the procedure is performed in a sterile theatre. The wound site may become red, hot and painful. There may be a discharge of pus or fluid. This is usually treated with antibiotics and an operation to washout the joint may be necessary. In rare cases, the implant may be removed and replaced at a later date (revision surgery). The infection can sometimes lead to sepsis (blood infection) and strong antibiotics are required.
Rare
- Pulmonary Embolism – This happens when a blood clot (DVT) breaks off and lodges within the lungs. It can affect breathing and is a serious condition that can be fatal.
- Poor scars – The wound may become red, thickened and painful (keloid scar); this is more common in Afro-Caribbeans.
- Nerve Injuries – Efforts are made to prevent this, however damage to the small nerves of the knee is a risk. This may cause temporary or permanent altered sensation or movement around the knee and lower leg. It is common to have a patch of numbness to the outer aspect of the knee, this generally resolves with time.
- Fracture – Bone may be broken when the new implant is inserted. This may require fixing immediately or at a later date.
- Instability – Rarely the reconstructed joint can be unstable and this can require further surgery.
- Blood vessel injury – Blood vessels at the back of the knee may be damaged, this can require further surgery by the vascular surgeons.
- Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop. 2017;41:2265-2271.
- Batailler C, White N, Ranaldi F, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. European Society of Sports Traumatology, Knee Surgery, Arthroscopy (ESSKA) 2018.
- Jaramaz B, Nikou C, Casper M, Grosse S, Mitra R. Accuracy validation of semi-active robotic application for patellofemoral arthroplasty. Paper presented at: International Society for Computer Assisted Orthopaedic Surgery; June 17-20, 2015; Vancover, Canada.
- Jaramaz B, Mitra R, Nikou C, Kung C. Technique and Accuracy Assessment of a Novel Image-Free Handheld Robot for knee Arthroplasty in Bi-Cruiciate Retaining Total Knee Replacement. EPiC Series in Health Sciences. 2018;2:98-101.
- Gregori A, Picard F, Lonner J, Smith J, Jaramaz B. Accuracy of imageless robotically assisted unicondylar knee arthroplasty. Paper presented at: International Society for Computer Assisted Orthopaedic Surgery; June 17-20, 2015; Vancover, Canada.
- Ponzio DY, Lonner JH. Preoperative Mapping in Unicompartmental Knee Arthroplasty Using Computed Tomography Scans Is Associated with Radiation Exposure and Carries High Cost. J Arthroplasty. 2015;30(6):964-967.
